Can you have both adhd and autism? Understanding Dual Diagnosis
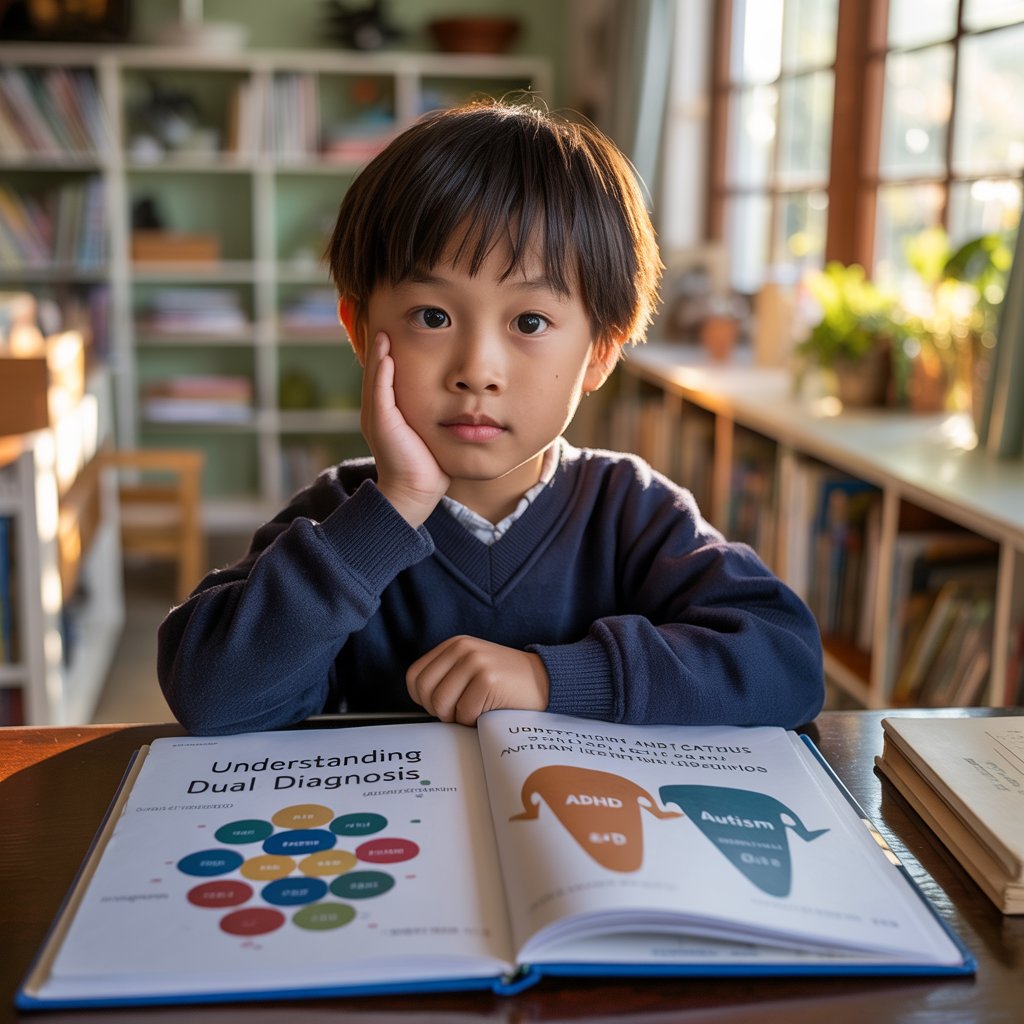
Ever wonder why your brain seems to work in two different operating systems at once? You're not alone. Many people live with both ADHD and autism spectrum disorder (ASD), a combination that creates a unique neurological profile that's greater than the sum of its parts.
I've worked with hundreds of clients navigating this dual diagnosis, and I'll tell you—understanding how ADHD and autism interact changes everything.
This isn't just about checking boxes on a diagnostic form. It's about recognizing how these conditions blend together, creating challenges and strengths that don't fit neatly into either category alone.
But here's where it gets interesting: the overlap between these conditions can make diagnosis tricky, even for experienced clinicians. So how do you know if you're dealing with one, the other, or both?
The Overlap Between ADHD and Autism: Facts and Statistics

The rising prevalence of dual diagnosis in recent years
Picture this: Ten years ago, most kids got either an autism diagnosis or an ADHD diagnosis - rarely both. Fast forward to 2025, and the landscape has completely changed. Dual diagnoses of ADHD and autism have jumped by nearly 50% in the past decade alone.
Why the dramatic increase? It's not necessarily that more people suddenly have both conditions. Instead, our understanding has evolved significantly. Clinicians now recognize that these two neurodevelopmental conditions can and often do occur together.
The DSM-5-TR (updated in 2022) officially allows for concurrent diagnosis of these conditions - something that wasn't possible before 2013. This change alone has opened the door for more accurate diagnoses and better support for those who experience both sets of challenges.
How common is the co-occurrence of ADHD and autism?
The numbers are genuinely eye-opening. About 50-70% of individuals with autism also meet the criteria for ADHD. Going the other direction, roughly 15-25% of people diagnosed with ADHD also have autism.
This isn't just happening in adults. Studies looking at children diagnosed with autism found that over half show significant ADHD symptoms too. Many families discover this overlap when treatment for one condition doesn't fully address all their child's challenges.
Diagnostic RelationshipPercentageAutism patients who also have ADHD50-70%ADHD patients who also have autism15-25%
These statistics shouldn't be shocking when you understand the underlying connections between these conditions.
Research findings on the genetic and neurological connections
Dive into the brain scans and genetic studies, and the overlap starts making perfect sense. Both conditions share certain genetic markers - particularly mutations affecting dopamine regulation and neural development.
Brain imaging studies reveal similar patterns of connectivity issues in certain regions, especially those involving executive function and social processing. The prefrontal cortex, basal ganglia, and cerebellum show parallel differences in both conditions.
A landmark 2023 study published in Nature Neuroscience identified specific gene expression patterns that create a sort of "neurological Venn diagram" between the two conditions. These shared genetic factors explain why they so frequently co-occur.
Simply put, ADHD and autism have overlapping biological roots. Think of them not as completely separate conditions but as different manifestations of related neurological variations.
Why dual diagnoses were historically overlooked
Up until 2013, you literally couldn't be diagnosed with both conditions simultaneously. The old DSM-IV guidelines explicitly prohibited it. Clinicians had to choose one or the other, often picking the diagnosis that seemed most prominent.
This created a massive blind spot in understanding. Symptoms of one condition were often misattributed to the other, leading to incomplete treatment approaches and confusion for patients and families.
The historical separation stemmed from outdated views about neurodevelopmental conditions. Medical professionals used to view autism and ADHD as fundamentally different types of disorders, rather than related conditions with overlapping features.
Training for specialists reflected this divide too. Autism experts and ADHD experts often worked in separate fields with little crossover in their education or practice. Many clinicians specialized in one condition and had limited expertise in the other.
The result? Countless people received incomplete diagnoses and support that addressed only part of their lived experience.